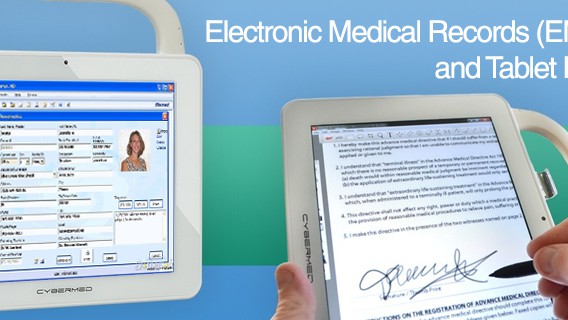
Electronic medical records (EMR) systems handle everything from documenting patient data and scheduling appointments to filling prescriptions and verifying insurance. You can do all this and more on a medical-grade computer or tablet, unlike older systems and their paper-filled files and folders.
Today’s post covers the benefits of implementing an EMR system throughout your medical group or organization. We provide stages of EMR implementation to guide in:
- Selecting and preparing the EMR software
- Ensuring compliance with privacy and security regulations
- Training the organization’s care team
- Troubleshooting any issues that may arise
What Is Electronic Medical Record Implementation?
Article Guide
An electronic medical record is a digital version of a patient’s chart. The first EMR system went live in 1972, and its successors have brought a major digital transformation in healthcare.
EMR implementation is the process of moving your medical practice or group’s paper-based patient record system to a software system. It can also mean moving from your old software to a new one.
Healthcare organizations implement electronic medical records to deliver a modern standard of patient care.
Use Cases for Electronic Medical Records
Five major use cases for EMR involve:
- Patient charting: Providers and medical staff can easily access a patient’s complete medical history in any connected medical computer. Updates can be made and viewed in real time.
- Remote patient monitoring and assisted care: Providers can get real-time updates on a patient’s condition whether the patient is at home, in an assisted-living facility, or other remote location.
- Medical lab connectivity: A patient’s latest blood tests, X-rays, and pathology reports can be pulled up immediately in an EMR for review.
- Medical prescription: Medications can be sent to a patient’s primary pharmacy with the touch of a button.
- Billing forms: All billable transactions are in one location for the accounting and financial departments to review and charge appropriately.
Benefits of EMR Implementation
These use cases hint at the benefits of EMR systems, which revolve around higher quality of care, improved patient outcomes and safety, and enhanced communication between patients and providers.
These benefits include:
- Saving space: EMR systems save on space and reduce operational costs by keeping records in one place. Medical offices and clinics won’t need to store, manage, and retrieve paper records, which can be scattered throughout a medical facility.
- Optimized workflows: An EMR system reduces unnecessary or redundant work while keeping track of patients and their visitors. This frees up valuable time for the staff members to focus on other, more vital duties like caring for the patients.
- Error reduction: EMRs help reduce errors during documentation, such as misspellings of a patient’s name or medication. They can also alert providers if treatments conflict with each other or prevent repeat tests by letting the provider know if a particular test has already been ordered. All these measures improve patient care.
- Greater accessibility: Multiple providers can view a patient’s EMR simultaneously as long as they have permission. This allows medical teams to work from the same page in complicated procedures like organ transplants.
How Long Does EMR Implementation Take?
How long an electronic medical record EMR system implementation will take depends on numerous factors and variables.
A mid-to-large healthcare organization can implement a new electronic medical record system within a year. You can shorten this figure to six to nine months if you’re just updating your current system.
A solo practitioner or small medical group may implement their EMR system in six to nine months. Some may be able to do so in only a few weeks. Again, it depends on the factors and variables involved.
Eight Steps for a Successful EMR Implementation
Implementing an electronic medical record EMR system takes significant planning, collaboration, and coordination. You and your healthcare IT team will want to ensure the implementation plan is fleshed out as much as possible. When done right, a new EMR system can significantly increase patient care quality while keeping costs the same or even reducing them.
We provide the following eight best practices and steps with action items to guide your organization’s successful EMR implementation.
1. Plan an EMR Implementation Roadmap
The first step is to create a checklist of all necessary tasks, including establishing:
- Who are the stakeholders?
- What’s the budget?
- What are the exact features you’ll want in the EMR system?
These – and a lot more – are just some questions to ask as you and healthcare IT brainstorm the checklist.
An excellent place to start on your roadmap is deciding if EMR implementation will be done in a modular fashion or step by step:
- The modular approach breaks tasks down into smaller and simpler subtasks that are independently worked upon by different people and teams.
- Step-by-step fully completes each task before going on to the next one.
After deciding on your approach, follow these steps as you aim to successfully implement an electronic medical records system.
2. Define Your Budget
When budgeting, remember you want your EMR system to increase the quality of healthcare services while lowering costs. There are too many examples of healthcare organizations overspending during EMR implementation with little return to no return on the investment.
The Healthcare Financial Management Association developed a sample plan for an EMR implementation budget. Notable line items include:
- Human resources expenses (training and consultancy)
- Supplies (system upgrades)
- Administrative costs (training fees)
The budget will be primarily determined by your organization’s size and the selected EMR software.
3. Appoint Strong Project Leaders
EMR implementation is complex and far-reaching. You’ll need a team to ensure each process and task is done on time and within the budget.
Typical members who compose such a team include:
- Project management /practice manager – manages the EMR implementation, including post-rollout testing
- Application analyst – responsible for the EMR’s data migration and cleansing
- Application developer – customizes the EMR system
- QA test engineer – responsible for EMR system testing and performance
- Physician advocate – gives provider’s view on the software’s training, data, and testing
- Nurse advocate – provides nurse’s view on the software’s training, data, and testing
- Billing advocate – represents the billing department’s viewpoint on the software
All members must work closely to ensure the EMR software functions as intended.
4. Select the Right EMR Software
Selecting the right electronic medical record is one of the most challenging steps you and your implementation team will make. EMRs are complex programs with multiple capabilities and features. You can’t test-drive one after the other, like when shopping for a new car.
To narrow your choice, do the following:
- Clarify your EMR system priorities:
- Cost control
- User-friendliness
- Cloud-based hosting
- Implementation and training
- Integration with current systems
- Customer service
- Obtain an EMR certification from the Office of the National Coordinator for Health Information Technology.
- Obtain Requests for Information (RFI) and Request for Proposals (RFP) from EMR vendors. Their system must be HIPAA compliant. If not, immediately disregard their RFI and RFP.
- Have your team evaluate the RFIs and RFPs. How well do they match your goals?
- Create a shortlist of the top three to four vendors.
- Bring in the vendors to demonstrate their systems. Ask questions. Example: Is there an optimal medical-grade monitor that works with the EMR?
- Finally, select your vendor.
5. Prepare Your Technology Infrastructure
In this step, your team will prepare the various components of your medical office or healthcare group’s networks to handle the EMR system.
Is there enough processing power to work effectively with the software? “Processing power,” in this case, can range from data lines to wireless connectivity and storage space for cloud-based EMR systems.
Evaluate all involved hardware. Do the medical-grade computers have features like RFID identification to verify user identity? The patient health records in EMR systems are protected by law. The more robust your security protocols, the easier to stay compliant.
Your group’s healthcare IT and the EMR implementation team can ensure the infrastructure is ready for the new system.
6. Test and Troubleshoot Your System
The group’s infrastructure is ready. It’s time to migrate or transfer the information from your previous medical record system.
- Prepare the migration strategy. What needs to be transferred? Which fields? Have a backup strategy in case issues arise with the new EMR.
- Convert paper records into electronic ones.
- Clean and verify the data.
- Set up the EMR database.
- Migrate data to the new system.
- Test and verify that all old and newly entered medical data and records are correctly placed.
7. Train Your Users
An EMR system only works if its users understand how to apply its features correctly. You should schedule training programs throughout the organization shortly before the new EMR goes online.
- Training can be self-paced and on-site instruction. Self-paced has staff members reading user guides and watching instructional videos on the EMR’s numerous features.
- On-site instruction has an instructor, usually brought in by the vendor, come to the workplace to teach users.
You will need to determine which method is preferable based on your group’s workflows and availability of personnel.
8. Make Continuous Improvements
EMR implementation is not finished once the system is live. This last step has you and your implementation team evaluating the software to ensure it meets your goals. Consider:
- Assessing profitability using ROI calculations.
- Ensuring prompt and thorough data entry by evaluating data error rates.
- Gauging the impact on the quality of care through patient interviews.
- Measuring provider satisfaction through surveys.
Once you’ve received the above information, look for ways to optimize those areas.
Make EMR Implementation a Breeze with Cybernet Computers
Electronic medical records are essential to today’s modern healthcare, simplifying many workflow issues like error reduction and prescription refills.
EMR software systems are understandably complex given their numerous functions, which can make EMR implementation daunting. However, with a proper roadmap, robust implementation team, and step-by-step plans, medical groups like yours can successfully implement EMR systems with minimum disruption.
Contact a Cybernet team professional if you’re looking to implement EMR software from your medical office to a healthcare organization. Our professionals know how our medical-grade PCs, tablets, and medical box PCs fit during implementations.
Built from the ground up to work in the most demanding healthcare environments, they’re ready to house your EMR software with security features like Imprivata Single Sign-On and compatibility with legacy medical devices and equipment.
Connect with us on this and other relevant topics by following us on Facebook, X, and Linkedin.
Electronic Medical Records (EMR) and Tablet PCs
October 1, 2015
Physicians are very busy in any healthcare setting. They go from room to room without a moment to spare. Patients can end up waiting for hours. How much of a relief would it be if they had a piece of technology that…
0 Comments5 Minutes
You Can't
Learn from a Pop-up
But we can deliver knowledge to your inbox!
We dive deep in the industry looking for new trends, technology, news, and updates. We're happy to share them with you.
Knowledge, News, and Industry Updates Right in Your Inbox