In the mid-Fifties, computer use in hospitals was mainly in the automation of financial and accounting tasks. As the technology grew and regulations such as HIPAA (Health Insurance Portability and Accountability Act) and Medicare/Medicaid information systems changed, computers became more and more common in other parts of medical facilities.
Today, medical computers are found everywhere in healthcare. We’ll be covering five uses in hospitals.
Tracking Patient Health (EHR)
Article Guide
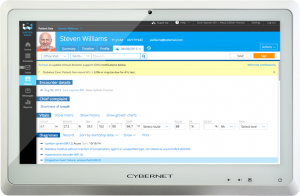
An electronic health record or EHR is a digital version of a patient’s paper chart. Early EHR efforts started in the 1960s and 1970s in academic medical centers. The 80s saw the introduction of industry-wide standards to make them more widespread.
The US government accelerated the trend in the 2000s. The HITECH Act of 2009 offered higher payments to healthcare providers who met “meaningful use” criteria with EHR. This was further encouraged in 2011’s Medicare and Medicaid EHR Incentive Program.
The impact on healthcare groups and hospitals was dramatic. Providers and medical staff in the past typically wrote notes on paper when examining patients. The move to computerized systems virtually eliminated this paper-based record-keeping. This resulted in improved efficiency and effectiveness as doctors and nurses could enter pertinent information on the spot instead of trying to recall it later. EHR also eliminated a lot of potential for mistakes like pharmacists trying to read the doctor’s handwriting.
Today, over 90 percent of healthcare groups are using EHR programs. Many run them on medical computers since they are optimized for the software. Common features found among these machines include:
- All-in-one design and touchscreen. This keeps the amount of equipment to a minimum so both medical staff and healthcare IT can focus on patient healthcare instead of hardware issues.
- Screen sizes range between 19” – 24”. This makes it easy to see all the important patient data with minimal scrolling depending on the EHR software. This can help prevent doctor burnout and resignation.
- Medical grade. This is an international standard for electromagnetic and radiation emissions that determine whether or not an electronic device is safe for near patient use. Computers that are medical grade will not interfere with critical medical devices like anesthesia machines. Providers and medical staff can update patient medical records in the OR or ICU without concern.
Patient Monitoring In and Out of Hospital
In the past, medical staff such as RNs, CNAs, etc. would periodically go into a patient’s room and check their vitals. Now patients admitted to a hospital are attached to machines that allow heart rate, respiratory activity, blood pressure, and other critical vital signs to be collected automatically in digital formats. The computers used can notify the staff when any of these statistics fluctuate from particular limits. The patient’s breathing becomes irregular is one such example.
Such monitoring can also be done remotely thanks to telemedicine. Hospital staff can monitor patients’ vitals while they rest comfortably at home or in a nursing facility. Staff can alert the patient directly, their provider, or first responders if there’s an issue. This is a boon for patients located in rural and other hard-to-reach places.
Hospitals have found numerous advantages using medical computers for patient monitoring. Being medical grade means they won’t interfere with the medical devices monitoring the patients. Computers built with an antimicrobial* resin baked in their casing to protect the computer casing from deterioration and degradation. While an IP65 rating makes them waterproof for easy cleaning and disinfection by staff.
Fanless design in medical computers has also proven a useful feature for patient monitoring. As its name implies, fanless computers don’t use fan blades to keep cool. This prevents the circulation of any airborne pathogens in the hospital room or even in a patient’s home. They also don’t make any noise which helps patients rest and recover more quickly and thoroughly.
Remote Diagnosis by Telemedicine
Telemedicine is the use of electronic information and communication technologies to deliver health care services from a distance. This can range from calling the on-call nurse for advice on a colicky baby, to a ship crew using real-time video conferencing to speak with a physician who is based on land. The technology saw enormous use and growth over the past couple of years due to COVID-19.
Hospitals use telemedicine in several ways:
- Care of patients with chronic conditions such as diabetes or hypertension. They usually need to see their doctor regularly. Now providers can discuss their conditions via telephone or video instead of periodic office visits.
- Allow physicians to contact patients remotely. This is especially useful for those who live in rustic zones with restricted medical services alternatives like no nearby medical offices.
- Communicate via computers and smartphones with colleagues from all over the world. Primary care providers can offer specialty care, such as cardiology or neurology, to patients even if the specialist is hundreds or even thousands of miles away.
Hospitals like medical computers for telemedicine since many have already been built with the technology in mind. Many have built-in front-facing cameras and microphones to make communication easy with patients and providers. This is important since providers will be making their diagnosis based on what patients tell them and what they can see on the screen. Large screens also make it easy to use EHR (see above), while fanless design means no distracting fan noise during conversations.
Mobility Moves Computers, Not Hospital Staff
Past computers used in hospitals were stationary setups composed of monitors, keyboards, and possibly a computer tower (if a PC). After seeing the patient, staff had to find these setups and re-enter their written notes.
Today, computers move with the hospital staff.
Workstation on Wheels
Computers can now be mounted on special carts called workstation on wheels or WoW. These can be moved around the hospital as needed by staff. An RN can enter a patient’s room, input their information in the EHR, then move onto the next patient. Later, a provider can take the WoW for their own use.
Medical computers are built to work in conjunction with WoW. While many WoW carts have batteries to provide power to their computers (“powered carts”) , the vast majority do not.
Medical computers with hot-swappable batteries work with such non-powered WoW. They have removable batteries that can be recharged as needed. This makes the entire setup lighter since there’s no heavy battery attached to the WoW. It’s also less expensive.
There’s another advantage. A powered WoW has to be periodically recharged. This takes its computer out of use for many hours. Medical computers with hot-swappable batteries have no such limitations since their depleted batteries can be quickly exchanged with a fresh one. This allows them to handle being on 24/7, which is a typical hospital schedule.
Medical Tablet
Today’s hospital staff are literally carrying their computers with them thanks to tablets. With these portable PCs, medical personnel can move about the various departments and enter whatever information is necessary. Providers at a patient’s bedside, for example, can review their notes and order lab work on the spot and in real-time. Other medical staff can pull up that information for other purposes like billing.
Medical tablets in hospitals have been proven to have many advantages over off-the-shelf models. They are medical grade which means they can work around patients and their medical devices safely. Many have antimicrobial* properties protect the computer casing from deterioration and degradation, and are IP65 rated, which makes them easy to clean. Those built with industrial components allow them to survive accidental drops and bumps as well as function 24/7. This last ability is further enhanced on tablets with hot-swappable batteries.
Taking Inventory
Asset management is an important part to the success of any hospital. It has to make sure that all its equipment, supplies, and other such materials are accounted for.
Hospitals have turned to computers to help. These use real-time medical inventory software systems to monitor inventory levels instantaneously, allowing for more efficient ordering and reordering of supplies. This in turn helps the hospital reduce costs, maintain stock levels, improve patient safety, and optimize staff workflow.
Hospitals are using medical computers for this important task. This is because their hardware and software are already fine-tuned for the setting. Medical tablets, for example, used in the central sterile supply department have antimicrobial* casings protect the computer casing from deterioration and degradation. They’re medical grade, which means they won’t interfere with any delicate equipment in the department, and are made with industrial parts for near continuous use. Finally, such a tablet can be equipped with a built-in RFID scanner to make inventory scanning, recognition, and tracking a breeze.
Closing Comments
The introduction of computer technology into the healthcare industry has resulted in many great changes. Many can be seen in hospitals where medical computer use has impacted everything from recording keeping to inventory management.
If your medical group or hospital wants to know more about the advantages of medical computers for your hospital, contact a representative from Cybernet. As a true device manufacturer, Cybernet can customize products to meet your specific needs in a timely and cost-effective manner.
Also follow Cybernet on Facebook, Twitter, and Linkedin to stay up to date on this and other relevant topics.
3 Unique Point of Care Uses for Medical Computers
December 1, 2017
The term "point of care" may be a little bit unclear, so let's start off with defining what that means. Point of care testing suggests any medical treatment that can be done specifically where the patient is located.…
0 Comments6 Minutes
Best Hospital Settings for a Medical Computer
September 24, 2015
The importance of using medical computers stems back to when former Secretary of Health and Human Services, Mike Leavitt, noted the importance of effective information technology in hospitals. Levitt, who served in the…
0 Comments5 Minutes
4 Medical Devices that Absolutely Need Integrated Medical Computers
April 9, 2019
The days of enormous computers and huge medical devices are nearly over — as technology advances, it shrinks, and in no field is that more useful than in healthcare. Smaller tech means more mobile and agile medical…
0 Comments8 Minutes
You Can't
Learn from a Pop-up
But we can deliver knowledge to your inbox!
We dive deep in the industry looking for new trends, technology, news, and updates. We're happy to share them with you.
Knowledge, News, and Industry Updates Right in Your Inbox





