Medical workers are highly-skilled, educated professionals in the highest demand they’ve ever been, and the hospital of the future is the one that respects and preserves their precious time.
To create the hospital of the future, modern medical organizations need to invest in the software and solutions of the future. Medical transcription is one such tool, and it must evolve to save staff time, facilitate accurate EMR, and bolster data insights to help do what medicine does best: create healthier patient outcomes.
Medical transcription has already started moving away from manual transcription of traditional audio notes into digital note taking, voice recognition, and machine learning transcription.
We’re going to show you how medical transcription is changing, how modern methods are tackling the solution, and how to prepare your staff and equipment for what the future will bring.
Manual medical transcription is on a slow but steady decline
Article Guide
Manual medical transcription will likely have a role to play in the next ten years or so, but the numbers are showing a continuous employment drop-off in the face of automated software.
The Bureau of Labor Statistics puts the current number of medical transcriptionists in the US at 52,400. By contrast, there were 57,400 medical transcriptionists in 2016, which shows a yearly average loss of about a thousand jobs a year.
Should automated transcription software become either cheaper or more reliable (or both), expect those numbers to fall faster.
Manual transcription also creates opportunities for HIPAA violations
As any medical professional (or medical lawyer) will tell you, part of the data-filled future of medicine is an increased focus on data security and HIPAA compliance. One of those easily-patchable security holes required for the future of medical transcription is the exporting of patient data to outside transcriptionists.
A medical transcriptionist vendor in New Jersey, “Best Medical Transcription,” and the medical group that contracted with it were fined over half a million dollars for mishandling the medical notes of over 1,600 patients.
These medical notes belonged to the patients of Virtua Medical Group, and were sent to “Best Medical Transcription” for, you guessed it, transcription. However, somewhere in the process, the notes and transcriptions were uploaded to an unsecured FTP website that literally anyone could access.
Worse, Google’s automated processes actually found the notes on the FTP server and indexed them into the search engine itself. For a time, the medical data of those 1,600 patients could be found with a simple Google search.
“Best Medical Transcription” was ultimately dissolved over the incident, with the owner himself having to pay additional fees and fines over the initial settlement.
Medical transcription software is getting bigger and better
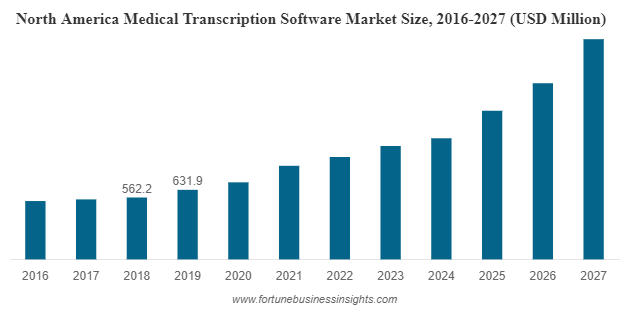
According to Fortune Business Insights, the medical transcription software market is predicted to reach 4.89 billion dollars by 2027. In 2019, that number was 1.32 billion.
This boom in automated medical transcription software can be attributed to a few notable developments:
- Advancement in voice recognition technology
- EMR and data-driven medical strategies increasing the demand for transcription
- Budgetary concerns creating a need for a cheaper and faster alternative
Advancement in voice recognition technology is making automated transcription more accurate. Voice recognition and dictation software have grown more accurate in recent years due to advancements in machine learning and AI.
Most transcription software these days claim a 99% level of accuracy (though, these numbers reflect perfect lab conditions and not the complexities of human voices recorded in the real world).
EMR and data-driven medical strategies increase demand for automated voice transcription. More stringent record systems and a greater focus on data-driven insights means more typing for doctors and other medical professionals.
Unfortunately, a study found that the average typing speed for doctors in training was found to be around 30 words per minute. Doctors and other medical professionals already believe they spend too much time at the computer (16 minutes per patient, in fact) due to EMR. However, automated transcription software allows doctors to dictate their notes and have the text auto-generated. If you’re not seeing the cost benefits, consider this: the average American speaks at around 125 words per minute. Dictating is nearly five times faster than typing.
These time savings really only come to fruition with transcription software that can quickly and accurately turn those audio files into text. Which, due to tech advancements, we have now.
Tighter budgets have less to spend on manual medical transcription. The last reason for the success of medical transcription software has been simple economics. With hospital funds spread thin and less medical staff to do the work, automated medical transcription saves labor hours and the money spent on manual transcription.
Sure, automated software comes at a cost, but it can scale much more easily with very little increase of cost by volume.
Medical tablets will speed up and humanize note-taking
Medical transcription isn’t just the process of turning audio into text: it can also be the transcription of hand-written notes to digital text.
Traditionally, doctors and nurses took notes on paper during their visits with patients. Then, in-office computer stations took over, but they created a distance–the user is filling out digital paperwork with the monitor acting as a wall between doctor and patient. Or, worse, the doctor or nurse has their back to the patient completely. Necessary, but not ideal.
With specialty medical tablets, doctors and nurses eliminate the physical distance and can use a stylus to quickly jot down notes on the tablet itself during an office visit. Using natural language processing, medical tablets can turn that handwriting into digital text, and can even be programmed to know which fields of the EMR to fill in with those notes.
This method skips the audio-to-text process completely.
Ambient medical transcription software records notes on its own
The ultimate future of medical transcription might be software that detects medical and patient conversations and records them automatically and imports them directly into that patient’s EMR.
Called “ambient medical transcription” or “ambient clinical intelligence,” this software (developed by companies like Nuance and DeepScribe) uses AI and natural language processing to fully automate medical documentation.
With this software, you turn on the app on a medical professional’s phone, medical cart computer, or medical tablet. Then, these ambient medical transcription apps can work in the background to recognize, record, transcribe, and input all relevant medical data being discussed during the patient visit. The software even integrates with many existing EMR platforms.
Like medical tablets, this ambient transcription software allows doctors and nurses to be more personal, friendly, and conversational, since they don’t have to focus so much on the details of note taking and EMR.
These ambient transcription programs are also useful for the growing recording and medical transcription needs of telehealth.
Closing Thoughts
To prepare for the future of medical transcription, hospitals and medical offices will need medical-grade computers that can integrate hardware like mics and cameras with automated transcription software.
Reach out to an expert at Cybernet to learn more about how the features of specialized medical computers can dovetail with medical transcription software. Also follow Cybernet on Facebook, Twitter, and Linkedin to stay up to date on this and other relevant topics.
Medical Computers and the Hospital of the Future
May 27, 2021
With the advancements made in digital technology during the 2010s, we were already on the cusp of radical changes in medicine before COVID-19 hit. Now, things that just seemed like distant possibilities before have…
0 Comments10 Minutes
How Medical Computers Are Revolutionizing the Healthcare Industry
October 4, 2015
Medical computers manage patients’ information and allow functions like writing & tracking prescriptions, managing patient billing and tracking all aspects of a patient's medical care. Medical computers are…
0 Comments6 Minutes
Improve Interoperability with the Right Medical Computers
September 25, 2018
Every organization consists of different departments working in sync together to move forward. This is doubly true with healthcare organizations such as hospitals, which measure success in lives saved and patients…
0 Comments7 Minutes
You Can't
Learn from a Pop-up
But we can deliver knowledge to your inbox!
We dive deep in the industry looking for new trends, technology, news, and updates. We're happy to share them with you.
Knowledge, News, and Industry Updates Right in Your Inbox