With the proliferation of information technology, more and more healthcare organizations use some kind of electronic health record (EHR) to record and store information about patients and the treatment they receive. But how do we access and share this information between different providers, hospitals, or groups? The answer lies in embracing the principles of interoperability in healthcare.
What is Interoperability in Healthcare?
Interoperability is more than just a synonym for “communication,” although that is certainly a major part of it. Interoperability in healthcare refers to the collection of systems and practices that facilitate the seamless exchange, editing, and updating of medical information.
For example, let’s say a patient needs to be transferred from one hospital to another for more specialized care. With interoperability, both hospitals use the same EHR system and terminology when referring to the patient’s condition, health history, prior treatments, and more. This helps healthcare providers at the second hospital as they integrate the patient into their system and develop a treatment plan for them.
Types of Interoperability in Healthcare
Interoperability in healthcare occurs on several different levels, ranging from the language used by healthcare providers to describe various conditions and communicate with one another to the protocols for data storage and retrieval. Organizations that embrace interoperability at all of these levels will reap the greatest benefits.
Foundational (Technical)
Healthcare organizations rely on numerous systems for administrative and clinical tasks like billing, medication dispensation, documentation, and more. These systems must be able to communicate with each other within the organization and with external entities.
To facilitate communication, international organizations such as Health Level 7 (HL7) develop standards and guidelines, including the Fast Healthcare Interoperability Resources (FHIR). These resources provide an internationally recognized framework for sharing patient data, establishing a shared baseline for healthcare groups to communicate effectively with one another.
Just as important are EHRs and application programming interfaces (APIs). EHRs are a natural component of interoperability, as they can be digitally transmitted from one computer to another, making it easier for healthcare providers to work off the same information. APIs are used in the same way between computers, allowing them to share information between their programs with minimal human oversight.
Another technical consideration is hardware. Providers require medical computers that are powerful and reliable enough to support the healthcare sector. Only computers that have been independently tested and certified to standards such as IEC 60601-1 should be considered for this role, as consumer-grade PCs often lack the safety and reliability features necessary for healthcare applications.
Structural
One of the most common mistakes that occurs when working with large amounts of data is the creation of data silos. A data silo is a repository of data that is difficult for other groups within the same organization or collaborators outside that organization to access and work with. Healthcare, with its high requirements for security and reliance on specialized knowledge, is particularly vulnerable to forming data silos. A straightforward example is patient pharmaceutical records stored on a separate server or in a different format from the rest of the hospital’s records.
Data silos are a direct impediment to interoperability in healthcare, as they prevent providers from having a comprehensive understanding of a patient’s situation. Healthcare organizations must prevent silos from forming to ensure a steady flow of data, both internally and with external entities.
This need for openness must also be balanced with the need for security, as healthcare is one of the most frequent targets for cybercrime. Healthcare groups must implement secure and standardized methods of communication, such as Imprivata-based encryption to protect patient data and standardized protocols that help flag suspicious messages or requests.
Semantic
Interoperability in healthcare is impossible if providers don’t adhere to standardized language, such as SNOMED CT. As an internationally recognized collection of medical terms, SNOMED CT helps ensure that providers use the same language to describe the same conditions that patients might have. This prevents medical errors and ensures continuity of care between providers and facilities.
Similar semantic concerns exist for data. Healthcare data needs to be easily transferable from one model to another, such as taking a patient’s information from an EHR and moving it to another. This process is known as data mapping, and it saves providers time that would otherwise be spent manually filling out entry fields.
Organizational
Organizational interoperability refers to collaboration between different healthcare entities. This often takes the form of outside consultations or accepting patients who require more specialized care, ensuring they receive the best possible attention. Other organizations, such as housing, education, and criminal justice, can also benefit from collaborating with healthcare groups.
For example, during a pandemic, government agencies must be informed of how many citizens are infected and where hot spots for infection are, so that they can assign resources effectively. Similar to sharing between healthcare groups, however, measures must be taken to ensure patient privacy.
Advantages of Healthcare Interoperability
By embracing interoperability principles in their operations, healthcare groups can reap numerous benefits for both themselves and their patients.
Enhanced Patient Care
By utilizing EHRs and sharing information across all relevant stakeholders, providers can enjoy real-time access to a patient’s medical history and treatment plan, enabling them to deliver more accurate care. Because an EHR can be accessed on multiple platforms simultaneously, it also makes coordinating care across various providers easier than relying on a single set of paper records. A consistent source of seamlessly updated information also reduces the chances of medical errors occurring, as all involved parties work off the same knowledge base.
Increased Efficiency
With greater EHR implementation and data sharing, healthcare organizations can reduce the need for administrative tasks. This reduces payroll costs, enabling healthcare providers to focus on what truly matters: treating patients. EHRs also reduce the need for duplicate testing, which saves time, money, and stress for all parties involved.
Data-Driven Decision Making
Interoperability in healthcare also facilitates data-driven decision-making, which is crucial for effective large-scale population health management. By examining the health records of entire populations, healthcare groups can identify environmental factors that affect the community, such as pollution or disease outbreaks. Armed with information, both private healthcare groups and government agencies can act accordingly.
Obstacles to Interoperability in Healthcare
While an obvious benefit to all parties involved, implementing greater interoperability in healthcare does come with its own challenges. The most common hurdles to overcome are data security concerns, variations in standards and terminology, and budgetary issues. Thankfully, these problems also have solutions.
Data Security and Privacy
Cybersecurity continues to be an issue for healthcare organizations, especially when it comes to protecting the data and privacy of their patients. Following best practices for data security in healthcare, such as encryption and access control, is absolutely essential. This is doubly important for organizations pursuing interoperability, as any breach in their systems might also compromise those of their partners.
Inconsistent Standards and Systems
One of the most common roadblocks to interoperability is when healthcare organizations use inefficient methods of communication, such as different standards and terminologies. These inconsistent methods of describing the same condition or issue lead to misunderstandings, miscommunications, and medical errors that can seriously affect a patient.
Another significant issue on this front is the fragmented and often outdated nature of healthcare IT systems. Many hospitals and clinics still rely on proprietary systems designed and supported in-house. While these systems are sufficient for internal usage, they make collaboration with external entities incredibly difficult, as they cannot “talk” to the systems used by other groups. This forces healthcare groups to waste time transcribing information from one EHR to another.
Financial Concerns
Obviously, implementing new interoperable systems costs time and money. Staff need to be properly trained on how to use these new resources, and the new software needed to manage EHRs might not be compatible with older computers. Organizations need to budget appropriately and review what technology will be compatible with new tools and what will need to be replaced.
How to Stream Interoperability Adoption
While integrating interoperability into healthcare operations, there are ways to reduce that challenge. The best solutions for doing so include:
Adopt International Standards
As mentioned earlier, adhering to internationally recognized standards is a key step for achieving interoperability in healthcare. Doing so will make it far easier to communicate both internally and with other organizations.
Use Health Information Exchange Agreements
Health information exchanges (HIEs) are agreements between healthcare organizations that enable the seamless sharing of information between them. These information exchanges enable providers to treat patients more effectively, even if they aren’t at their normal site for care. California’s statewide HIE is an excellent example of this sample, coordinating healthcare for over 40 million people. Similar efforts to encourage collaboration between different stakeholders are critical and must be encouraged at every possible level.
Invest in Data Governance
With the exponential increase in the amount of data generated and used in healthcare, there is an equally exponential need for data governance. Healthcare groups must invest in dedicated IT professionals focused on governance and quality management to ensure that patient data remains accurate, secure, and accessible for the right people. They can also help prevent data silos from forming and ensure cooperation between various departments in the organization.
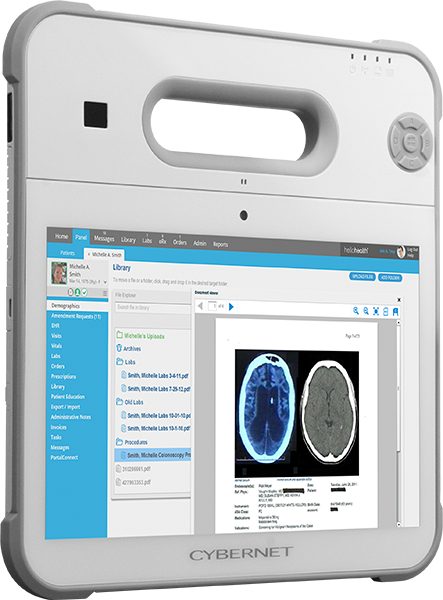
Embracing Healthcare Interoperability with Cybernet Manufacturing
By embracing interoperability in healthcare, organizations will be better equipped to treat patients, collaborate with other groups in the sector, and capitalize on new technological advances. While there are certainly challenges to overcome when updating procedures and tools, the benefits are too good to ignore.
If your healthcare organization aims to integrate interoperability into its structure, contact Cybernet Manufacturing. Our range of medical-grade tablets and computers is designed and certified specifically for healthcare environments, integrating features that make them ideal for interoperability, including RFID readers, barcode scanners, and compatibility with both modern and legacy equipment.