Electronic health records play vital roles in today's medical practice, from patient diagnosis to billing. That is why EHR implementation, or rolling out an electronic record system, is so important. But of equal importance, if not more, is optimizing such a system to the medical group's workflows, such as regularly updating patient records and scheduling follow-up appointments.
- What is EHR Workflow Optimization?
- Common Challenges in Current EHR Workflows
- Benefits of EHR Workflow Optimization
- Best Practices for Successful Implementation
What is EHR Workflow Optimization?
Electronic health records (EHR) follow a patient's entire medical history: diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results, to name a few. EHR workflow optimization aims to identify and resolve all the issues within the system to better meet the needs of healthcare providers, patients, and other stakeholders.
Common Challenges in Current EHR Workflows
Electronic healthcare records can be a challenge to implement and run effectively; unsurprising, given their capabilities and uses. Without proper workflow optimization, EHR systems introduce more issues and challenges to a medical group than they solve.
Routine Disruption
Improperly integrated EHR systems into existing workflows can disrupt routines as medical staff scramble to learn how to use them while still carrying out their regular duties.
Wasted Data Entry
Providers and other medical staff may find the EHR data entry process tedious and time-consuming, taking away valuable time from their patients. This could lead to dissatisfaction and burnout among providers, further straining patient care.
Interoperability Issues
Medical personnel may struggle to access patient records and information due to incompatibility with the group's various EHR systems or a lack of standardization, forcing them to search for the vital information through slower means.
Alert Fatigue
Too many improperly configured alerts and notifications from EHRs can lead to alert fatigue, in which the provider may start ignoring messages that are actually critical.
Usability Challenges
A poorly designed user interface for the EHR system is challenging for medical staff to quickly navigate and find a patient's record, where information – or a lack of it – is needed to deal with life-threatening situations (allergies, diabetic shock).
Data Accuracy and Integrity
Incorrect data, from misspelling the patient's last name to jotting down the wrong dosages of their heart medication, can affect their health care, ranging from annoying (wrong insurance bill) to dangerous.
Privacy Concerns
The patient data found in EHR systems is highly protected by regulations like the Health Insurance Portability and Accountability Act (HIPAA). Improperly configured EMRs may reveal such information to unauthorized personnel. Violations of these regulations can result in fines for the healthcare group or even jail time for staff.
Training Requirements
Medical staff who are not adequately trained with the EMR may become frustrated, leading to delays in patient treatment and strains on hospital budgets as vendor consultants and trainers are called in.
Resistance to Change
Providers and other staff may resist learning the new system, especially if they had no input in its selection and usage. Management may be forced to intervene, which could lead to ill will among medical personnel, lower morale, and potentially result in employee turnover.
Benefits of EHR Workflow Optimization
Optimizing EHR to a medical group's specific workflow brings out the technology's full potential for the users. The benefits are many.
- Clinical documentation, from patients' personal information to provider notes, is more accurate, easier to read, and track, thanks to reductions in human error typical in paper-and-file systems.
- Streamlined data entry and record-keeping processes allow providers to focus on giving quality patient care.
- Quick and easy access to medical records enables providers to see more patients daily, resulting in increased productivity and profitability.
- Collaborations among on- and off-site providers are made easy since EMRs are readily available through medical computer tablets and telehealth.
- Healthcare data security measures, such as biometric ID and data encryption, ensure patient data is secure and meets privacy standards and regulations.
- Storing EHR off-site and on the cloud can prevent data loss through cyberattacks and even extreme weather conditions like flooding.
- The EMR savings, in both time and money, are tremendous since there is no cost to print, store, and maintain paper files. Such savings can then be devoted to greater patient care.
Best Practices for Successful Implementation
A product of the healthcare sector's digital transformation, EHR replaced paper-and-file record-keeping with promises of more accurate patient information, instant searchability, and cost savings. Medical groups can make such promises a reality by implementing the following EHR workflow optimization strategies.
Audit Workflows
How does the medical staff use the EHR system? (This should primarily be aimed at the providers.) What specific forms are difficult to use? Can they bring up information easily? An EHR’s bottlenecks and workflow pain points should be noted and prioritized.
Leverage Built-in Features
What are the templates, macros, and order sets offered on the EHR? They can be configured to streamline workflows. More advanced systems come with dictation and speech recognition software to minimize data entry, which is always welcomed by providers.
Customize EHR Interface
The menus and shortcuts of many EHR systems allow for customization. Medical groups can use this to their advantage, prioritizing the features most often used by particular departments, for example.
Standardize Data Entry
Simply, ensure that information entered into the EHR is done consistently and in the proper format and terminology. This not only makes it faster for staff (and patients!) to enter and understand, but also minimizes errors and slow searches.
User Training and Support
Schedule training sessions for all involved staff, taking into account their work schedules to avoid overwhelming or discouraging them, especially when training how to use the advanced features. If the medical group is willing (and has the budget), consider having a dedicated support person available to answer questions about the EHR system and troubleshoot issues.
Integration with Other Systems
Healthcare interoperability refers to the ease with which various medical devices, equipment, and networks can exchange, edit, and update data. Check the EHR's interoperability to ensure it works with such technologies as lab systems and patient portals. Well-connected ones can avoid issues like double data entry, duplicate records, and a lack of record retrieval.
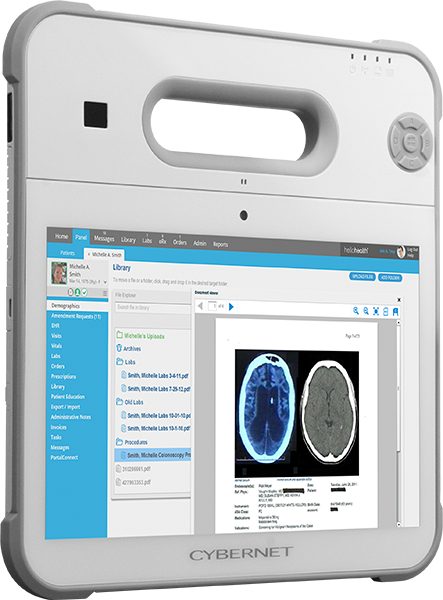
Keep Your EHR Workflow Optimized by Cybernet Computers
EHR workflow optimization aims to improve the functionality, efficiency, and usability of electronic health record (EHR) systems. By minimizing administrative burdens and reducing the risk of errors, an optimized EHR can improve a medical group's productivity, reduce provider burnout, and lower costs.
If you're looking for more information on EHR workflow optimization solutions, contact Cybernet Manufacturing. Our medical computers are purpose-built for EHR, with the hardware and software configurations to run your most demanding record demands with ease. Not finding what you're looking for with our pre-built? Not a problem! We're an original equipment manufacturer and have complete control of our PC designs and bill of materials. We're confident we can build the right computer, from an all-in-one PC to a medical AI computer, to your exact wants and needs.