You’ve been tasked by your healthcare group to submit recommendations for its electronic medical records (EMR) platform. You know the right (or wrong) EMR systems will have an impact for years to come, affecting medical staff productivity and the choice of medical computer to display patient records correctly. Today’s post provides some guidance for your research as it covers:
- EMR costs and features
- Popular EMRs on the market
- Details on Epic and why it’s widespread in the industry
How Much Does an EMR System Cost?
Article Guide
Between $15,000 to $70,000 and up to an eye-watering $500,000 and more.
If you are shocked by the wide range in these numbers, you are not alone. Comparing pricing information of EMR systems is a hard task. Most software is customizable based on the unique needs of the practice. Factors that go into them and their price tag may include:
- Type of storage chosen like on the clinic’s premise vs being cloud-based.
- Additional hardware costs like new arms and mounts for possible new computerware.
- Additional features like systems for technologists in the lab as well as radiologists and pharmacists.
- Associated costs for training on the system.
Healthcare groups looking to implement an EMR systems should take a hard look at the software and ask questions like:
Is it a generic system or one custom to your speciality?
Healthcare groups and their wide range of clinics and hospitals and clinics have led to a diverse market in EMR systems. This is unsurprising: a dental office will have different requirements than those in a major surgical unit.
Most systems break down into two types. Outpatient EHR systems are designed for use in small physician practices and similar, specialized centers like skilled nursing facilities. EHRs used here are often only used within a single department and rarely connect with others (i.e., have minimal or non-existent interoperability).
Inpatient EMR systems are the opposite. They are designed for use among multiple departments and have high interoperability with other on-site networks. This makes them perfect for most hospital settings.
What are its features?
Templates for patient information found in virtually all EMR systems include:
- Allergy information
- Demographic information
- Diagnoses
- Immunization records
- Lab test results
- Medication information
- Note
Applications for the following should also be asked depending, of course, on the medical practice:
- Integrations with coding and billing software.
- Telehealth capabilities.
- Care coordination.
If customizable, how easy is it to do so?
Is it easy for the medical staff to configure the EMR system to the group’s needs? Does healthcare IT (HIT) need to be brought in and trained? Or can the software be only updated by the company’s engineers? These are vital questions to answer. The more difficult it is to make the software work for HIT, the more costly in time and money it is to the group.
Just how easy is it to use the EMR software?
This is similar to the questions above. Is the system easy to figure out and use? Or will extensive training be necessary for even the most basic of functions? This question is of special importance to providers, nurses, and medical staff, whose schedules are chock full of patients. They rarely have the luxury of free time to learn the In’s and Out’s of unfamiliar software.
What’s the EMR system vendor’s policy?
This question asks what support will be expected by the vendor. Do they provide training to use their software? What are their hours of operations? Do they have a technician available during off-hours to answer questions or trouble-shoot the software?
Many healthcare software companies, in response to any and all of the above questions and more, won’t bring up figures until deep into the negotiations.
What are the Most Used EMR Systems?
The number of EMR systems is estimated to be 500 at the publication of this post. To help narrow down that figure to a manageable level, we provide two lists. The first one are the top 10 inpatient systems based on installs in hospitals as of 2022:
- Epic Systems
- Cerner
- Meditech
- Evident
- Allscripts
- Medhost
- Netsmart Technologies
- Athenahealth
- Harris Healthcare
- Indian Health Service
The second list is based off the winners for specific criteria:
- Allscripts: Best for large organizations
- athenahealth: Best for reporting
- Cerner: Best for multiple site organizations
- DrChrono: Best for medical billing
- eClinicalWorks: Best for telehealth
- Kareo: Best for small practices
- NextGen: Best for population health management
- RXNT: Best for multiple specialty practice
- TherapyNotes: Best for behavioral health practices
- Valant: Best for mental health practices
Is Epic the Most Popular EMR System?
“Popular” is a subjective term. What is not subjective is Epic will definitely come up a lot in discussions on EMR systems. This is especially true for inpatient use.
There is a good reason. Reports show Epic has a 32.9 percent share of US hospitals as of 2021. This figure rises to 58 percent when looking only at large hospitals (i.e., more than 500 beds). Also of note are which hospitals are using the EMR:
- Barnes-Jewish Hospital
- Cleveland Clinic Main Campus
- Fontana Medical Center
- John Hopkins Hospitals
- Stanford Hospital
- Massachusetts General Hospital
- Mayo Clinic Hospital
- Mount Sinai Medical Center
- New York-Presbyterian/Weill Cornell Medical Center
Reasons why healthcare groups choose Epic vary. What is know is that:
- Digital versions of a patient’s chart are interchangeably called EMR and EHR. However, the former usually stays in the patient’s healthcare group and doesn’t follow if they switch to a new one. An EHR, on the other hand, contains records from many groups and doctors and can follow the patient to a new group. Epic acts as both depending on the customer’s configuration.
- Epic has features for telehealth, billing, scheduling, and reports. It can work with both internal and external pharmacies to allow e-prescriptions
- The Health Insurance Portability and Accountability Act (HIPAA) aims to protect patient privacy. Epic has various built-in tools and features to keep patient data secure whether viewed on a mobile device (including Android, iOS and Apple Watch), a web browser, medical computer, or medical grade monitor.
- The Epic software platform is cloud-based which makes it easy to scale to the healthcare group’s wants and needs.
- Hospitals know Epic is currently the most popular choice as an EMR. Medical devices and equipment like medical grade monitors are optimized to display Epic records for ease-of-use by staff. That means they know they have little risk for incompatibility, lack of support, or company closure if they decide on the platform.
Closing Thoughts
Choosing an EMR system or systems for one’s healthcare group can be daunting. The costs range widely depending on one’s wants and needs, and even lists on which is “popular” vary greatly.
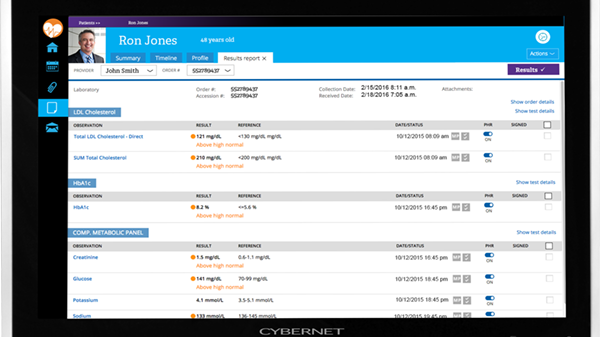
Contact an expert at Cybernet if you’re interested in learning more about EMR systems especially how medical computers and medical tablets are actually designed with them in mind.
Electronic Medical Records (EMR) and Tablet PCs
October 1, 2015
Physicians are very busy in any healthcare setting. They go from room to room without a moment to spare. Patients can end up waiting for hours. How much of a relief would it be if they had a piece of technology that…
0 Comments5 Minutes
Understanding How Medical Computers Enhance EMR Capability
June 6, 2018
Technology in hospitals has advanced greatly towards automation and electronic document storage to improve the lives of patients and facilitate the jobs of medical professionals. As of 2015 96% of all non-federal acute…
0 Comments7 Minutes
Why Personal Health Records are as Important as EHR and EMR
March 16, 2023
When most people hear of medical software, they imagine programs like electronic health records or telehealth. But it’s not just providers and healthcare IT who use them for the health industry. Patients are turning to…
0 Comments7 Minutes
You Can't
Learn from a Pop-up
But we can deliver knowledge to your inbox!
We dive deep in the industry looking for new trends, technology, news, and updates. We're happy to share them with you.
Knowledge, News, and Industry Updates Right in Your Inbox